Abstract
Whilst the addition of dexamethasone to upfront therapy with immunomodulatory (IMiD®) agents in myeloma (MM) is important to mediate rapid reduction in disease burden, preliminary findings suggest that the NK stimulatory effects of IMiD® compounds are best harnessed without the co-administration of dexamethasone. This may be especially effective in the setting of minimal disease burden (i.e. maintenance) when some inherent immune recovery has occurred, however this has yet to be confirmed in a prospective clinical trial.
Aims:
To evaluate the effect of maintenance with pomalidomide (POM) alone versus POM-low dose dexamethasone (LoDEX) following treatment with POM-LoDEX induction on progression free survival (PFS), overall survival (OS) and kinetics of response (overall response rate (ORR), clinical benefit rate (CBR)) in relapsed/refractory MM patients who were refractory to lenalidomide (R-LEN).
Methods:
MM14 was a multicentre, open-label, randomised phase 2 study of relapsed R-LEN MM patients who had received at least 2 prior lines of therapy. Patients commenced POM 4mg d1-21 (28d cycle) and LoDEX (40mg weekly). After 4 cycles (induction), patients with stable disease (SD) or better were randomised to receive POM alone (P) or combined with LoDEX (Pd) as maintenance. Therapy continued until toxicity/progression. All statistical analyses were performed using SAS software v9.4. The log-rank test was used to compare the survival distributions in the maintenance arms and pre-specified pointwise comparisons, with adjustment for multiplicity, were used to explore the possibility of non-proportional hazards.
Results:
154 patients from 11 Australian sites were enrolled (M:F 80:74), median age: 67yrs (range 35-88). Median number of prior treatment lines: 4.5 (2-14). All were R-LEN, 127 (82.5%) were bortezomib refractory (double refractory).
Median follow-up for all registered patients was 27.8m. Median PFS for all patients was 4.5m (IQR 2.3-8.3m) and median OS was 14.5m (IQR 6.7-30.7m). ORR was 40.9% (63/154); median time to achieve ORR was 4.6 months. CBR was 53.3% (82/154); median time to achieve CBR was 2.6m.
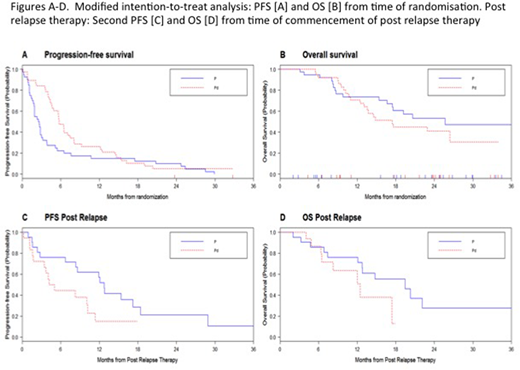
Eighty-one patients were randomised; however 3 were randomised in error. Therefore, a modified intention-to-treat (mITT) analysis included 78 (51%) patients who achieved ≥SD with induction and commenced maintenance: P = 40, Pd = 38. Median PFS (from time of randomisation) for P was 2.58m versus 5.73m for Pd (p=0.051) [Figure A]. Comparison of PFS at six 3-monthly intervals favoured Pd (from 3m to 12m) (p<0.00001), however at 18m, P was favoured (p=0.018). Median OS (from time of randomisation) was 25.6m for P versus 17.4m for Pd (p=0.356) [Figure B]. Comparisons of survival at six 3-monthly time points demonstrated no difference between the arms at months 3-12, however at 15m and 18m, survival favoured P (p=0.006 and p=0.02 respectively).
There was no difference in response (ORR, CBR) between P and Pd in the mITT population: ORR P (8/21) versus Pd (8/18), CBR P (12/21) versus Pd (11/18). In a landmark analysis for response achieved (ORR/CBR) at 4 months post registration, there was no difference in PFS or OS for patients within either arm according to whether they achieved ORR/CBR.
Of the mITT population (n=78), 39 had post-progression therapy data available (P = 21, Pd = 18). Of the remainder, 18 were palliated and 21 did not have available data. There was no difference in response (ORR, CBR) to salvage therapy between the two arms. However, responses were more durable for P compared to Pd: median second PFS (from start of post-progression therapy) was 12.7m versus 4.6m respectively (p=0.034) [Figure C]. P tended towards superior OS (from start of post-progression therapy): median 19.4m versus 12.5m (p=0.0922) [Figure D]. There was no difference in PFS/OS between individual treatment groups (bortezomib, carfilzomib, chemotherapy, thalidomide, LEN, other).
Conclusion:
After initial disease control with POM-LoDEX, MM patients continuing with POM-LoDEX had superior PFS compared to maintenance with POM alone. However, this early PFS benefit is lost and in fact reversed by 18m; and in those randomised patients who went on to receive post-progression therapy, more durable responses and superior survival were seen in those previously treated with POM alone. Correlative studies are underway to investigate the immunological mechanisms behind these observations.
Kalff:Janssen: Honoraria; Amgen: Other: travel to preceptorship; Celgene: Honoraria; Takeda: Honoraria. Reynolds:Novartis: Equity Ownership, Other: former employee of Novartis AG and holds stock in the company. . Quach:Amgen: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Janssen Cilag: Consultancy; Sanofi Genzyme: Research Funding. Ho:Amgen: Honoraria; Celgene: Other: Travel to meeting; Janssen: Honoraria; Novartis: Honoraria; Takeda: Honoraria, Other: travel to meeting. Mollee:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Estell:Janssen: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal